Gastroparesis is when your stomach has trouble emptying food properly. To manage it, you need to watch what and how you eat.
A gastroparesis diet emphasizes foods that are easy to digest. These foods can ease digestive symptoms and make sure you get enough nutrients, which is important for preventing flare-ups. For more detailed guidance on managing gastroparesis through diet, as well as exploring additional diets for health or weight loss, visit DietHCG.

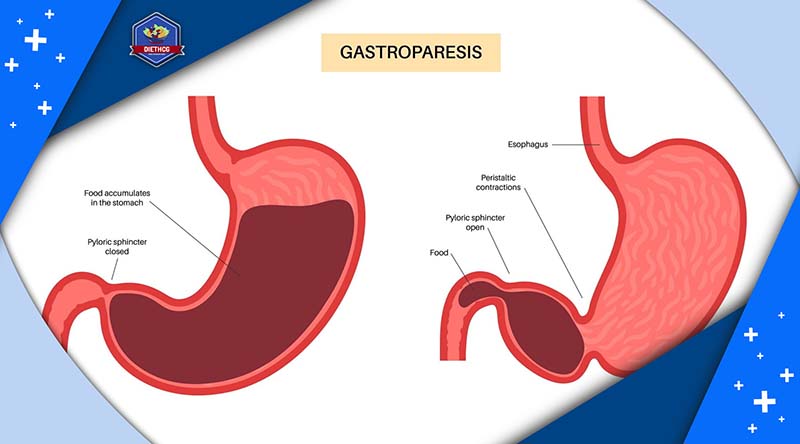
1. What Is Gastroparesis?
Gastroparesis, also known as delayed gastric emptying, is a condition where the movement of food from your stomach to your small intestine slows down or stops altogether. Typically, after you eat, the muscles in your stomach walls break down the food into smaller pieces and move them into your small intestine for further digestion. However, with gastroparesis, these stomach muscles don’t function properly, causing food to remain in the stomach for too long. This delay in digestion can result in a range of symptoms and potential complications.
2. What Is Gastroparesis Diet?
Typically, robust and spontaneous muscle contractions move food smoothly through the digestive system. However, in the case of gastroparesis, the stomach’s ability to contract is significantly slowed, hindering complete emptying.
Following a gastroparesis diet is the primary approach to managing this condition post-diagnosis. This diet emphasizes easily digestible foods, which alleviate strain on the gastrointestinal system, lessening uncomfortable symptoms like nausea, vomiting, acid reflux, bloating, and abdominal pain.
Moreover, prioritizing nutrient-rich foods helps the body cope with periods of reduced appetite often experienced during flare-ups. Neglecting proper nutrition during these episodes can result in malnutrition and unintentional weight loss.
Adhering to a gastroparesis diet may also enable individuals to avoid medications and other treatments associated with potential side effects.
3. Recommended Foods for Gastroparesis
If you’re managing gastroparesis, it’s vital to prioritize nutrition through frequent, small meals that are low in fat and easy to digest.
In this diet, focus on incorporating high-protein foods like eggs and creamy nut butter, along with easily digestible vegetables such as cooked zucchini. Choosing foods that are easy to chew and swallow can indicate they’ll be easier to digest.
Here’s a list of recommended foods that can help manage gastroparesis:
- Eggs
- Smooth or creamy peanut butter
- Bananas
- White breads, low-fiber or refined cereals, and low-fat crackers
- Fruit juice
- Vegetable juice (such as spinach, kale, and carrots)
- Fruit purees
4. Foods to Avoid with Gastroparesis
If you’re experiencing symptoms of gastroparesis, it’s crucial to know which foods to steer clear of.
As a guideline, limit consumption of foods that are high in fat or fiber.
Here’s a list of foods that could exacerbate discomfort associated with gastroparesis:
- Carbonated beverages
- Alcohol
- Beans and legumes
- Corn
- Seeds and nuts
- Broccoli and cauliflower
- Cheese
- Heavy cream
- Excessive oil or butter
5. Tips for Managing Gastroparesis Through Diet
To recover from a gastroparesis flare-up, consider following a phased diet plan that gradually reintroduces solid foods.
Though there are no official guidelines, a three-phase diet can be beneficial:
- First phase: Stick mainly to broth or bouillon soups and blended vegetable juice.
- Second phase: Progress to soups containing crackers and noodles, along with cheese and creamy peanut butter.
- Third phase: Include soft, easy-to-chew starches and softer protein sources like poultry and fish.
Throughout all phases, avoid red meat and high-fiber vegetables as they take longer to digest.
6. Conclusion
Adopting a tailored gastroparesis diet that includes eating small meals and moderating fiber and fat intake can help manage symptoms, regardless of its chronic or temporary nature. Consultation with a healthcare provider is essential to customize nutrition plans to individual needs, ensuring the body gets necessary vitamins and minerals for healthy organ function during gastroparesis recovery.


